Understanding the relationship between tone deafness and autism starts with defining tone deafness and exploring its connections to autism.
Defining Tone Deafness
Tone deafness, also known as amusia, refers to the inability to perceive or produce musical pitches accurately. Individuals who are tone deaf may struggle with distinguishing between different notes, recognizing melodies, or staying in tune while singing. This condition can impact a person’s enjoyment and participation in music-related activities, as they may find it challenging to grasp musical concepts.
Connection Between Tone Deafness and Autism
Research has shown that there is a notable overlap between tone deafness and autism spectrum disorder (ASD). Individuals with autism may exhibit difficulties in processing auditory information, including recognizing pitch and tone variations. This can manifest as challenges in musical perception and production, leading to a higher prevalence of tone deafness among individuals with autism.
Approaches for Addressing Tone Deafness in Autism
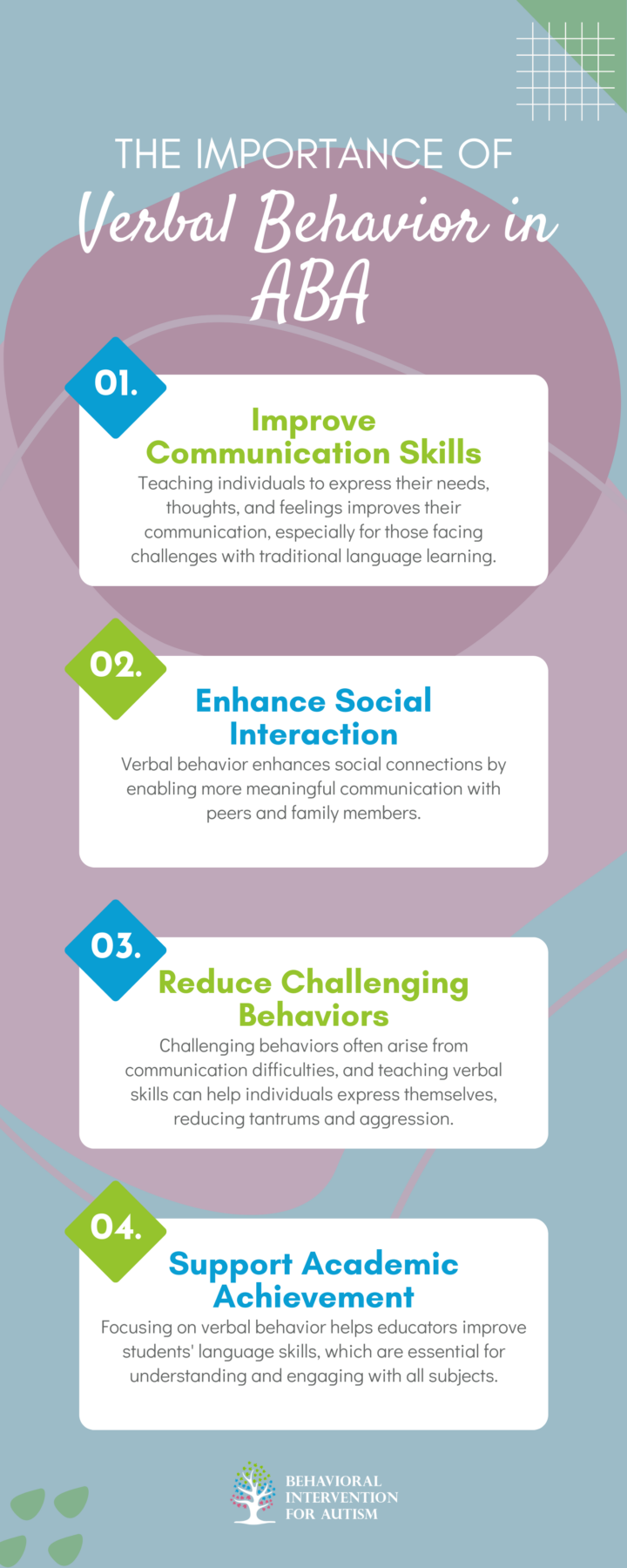
Addressing tone deafness in individuals with autism involves specific interventions and techniques to support their musical and communication development. The focus is on two main approaches: music therapy interventions and speech therapy techniques.
Music Therapy Interventions
Music therapy has been shown to be beneficial for individuals with autism who experience tone deafness. Through structured musical activities and interventions, individuals can improve their auditory processing skills, enhance their vocal expressions, and develop a greater sensitivity to different tones and pitches.
Music Therapy Intervention | Description |
Rhythmic Cueing | Using rhythmic cues to help individuals with autism stay in tune and synchronize their movements with music. |
Melodic Contour Training | Focusing on the shape of melodic lines to aid in recognizing and reproducing musical patterns. |
Pitch Discrimination Exercises | Engaging in activities that strengthen the ability to differentiate between different pitches, tones, and musical notes. |
Music therapy provides a creative and engaging way for individuals with autism to explore and improve their musical abilities while also addressing tone deafness in a supportive environment.

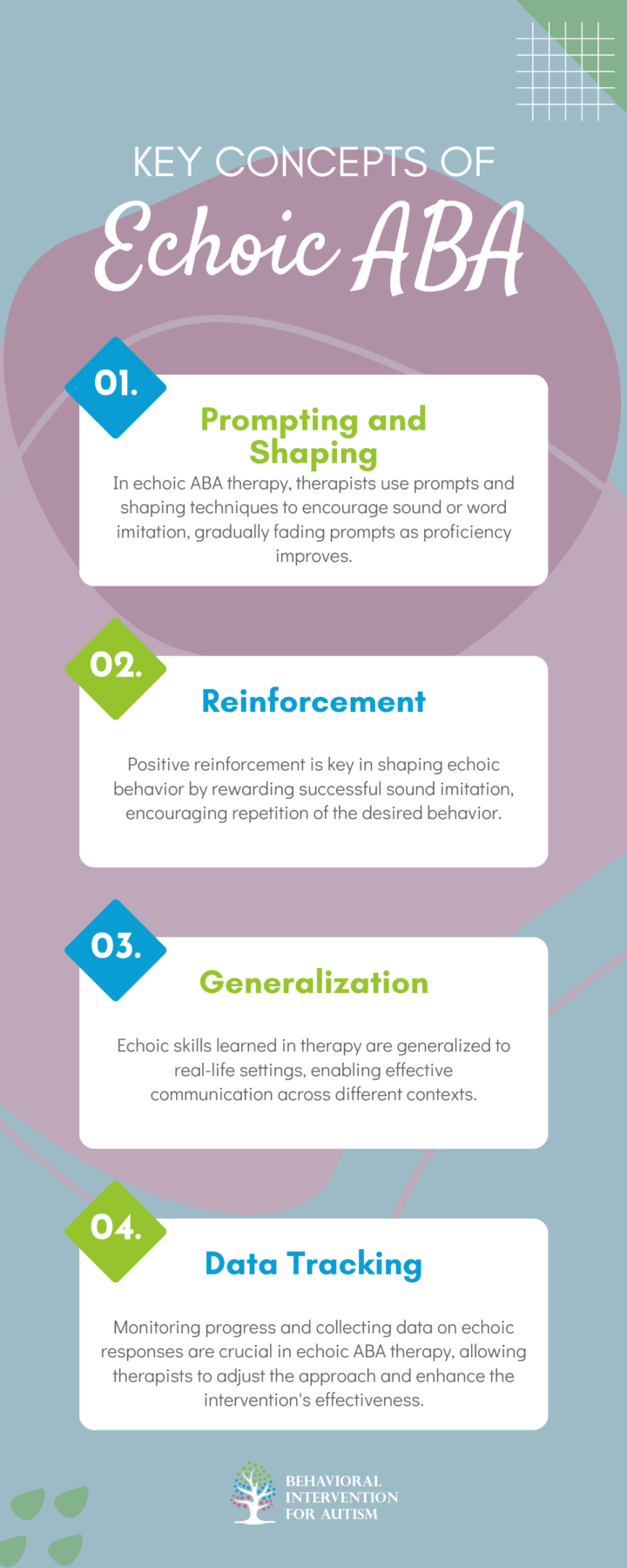
Speech Therapy Techniques
In addition to music therapy, speech therapy plays a crucial role in addressing tone deafness in individuals with autism. Speech therapists utilize various techniques to help improve vocal control, pitch modulation, and overall auditory perception in individuals with autism who struggle with tone recognition.
Speech Therapy Technique | Description |
Vocal Exercises | Engaging in vocal exercises that focus on pitch variation and control to enhance tone recognition. |
Ear Training | Practicing listening exercises to improve auditory discrimination and perception of different tones and pitches. |
Vocal Modeling | Using imitation and modeling techniques to help individuals replicate accurate tones and pitches in their speech and vocalizations. |
Incorporating tailored speech therapy techniques for individuals with autism and tone deafness can enhance communication skills, vocal expression, and tone accuracy in a structured and supportive environment.
Supporting Individuals with Autism and Tone Deafness
For individuals with autism who also experience tone deafness, creating a supportive environment and collaborating with professionals are key factors in ensuring comprehensive care.
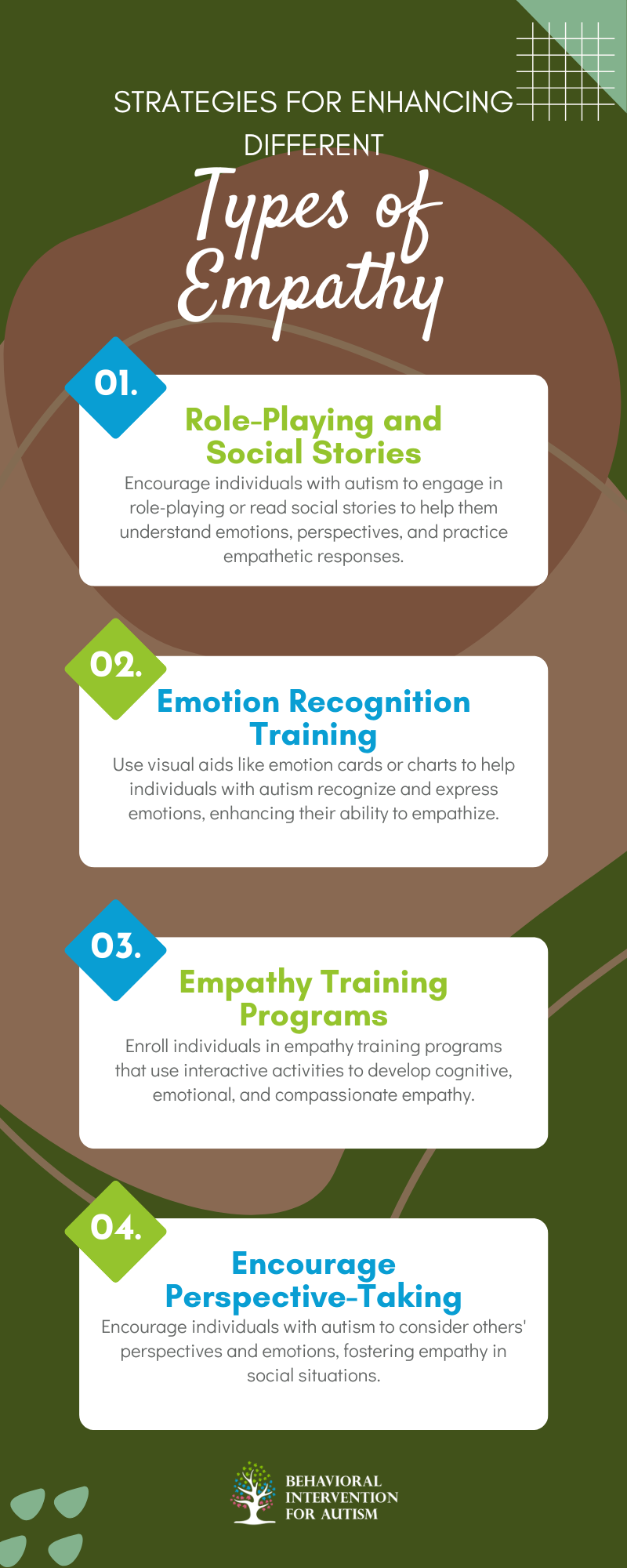
Creating a Supportive Environment
Establishing a supportive environment for individuals with autism and tone deafness involves tailored strategies to address their unique needs. Here are some approaches to consider:
Collaborating with Professionals for Comprehensive Care
Collaboration with a multidisciplinary team of professionals is essential for providing holistic care to individuals with autism and tone deafness. Here are some key professionals who may be involved in the care process:
Professional | Role |
Behavior Analyst | Conduct functional assessments, develop behavior intervention plans, and provide guidance on behavior management strategies. |
Speech-Language Pathologist | Assess and address communication challenges, including difficulties related to tone deafness, and provide speech therapy techniques to improve communication skills. |
Music Therapist | Offer music therapy interventions tailored to the individual’s needs, utilizing music as a tool for communication, emotional expression, and social interaction. |
Special Education Teacher | Design and implement individualized education plans (IEPs) that incorporate accommodations and modifications to support learning and development. |
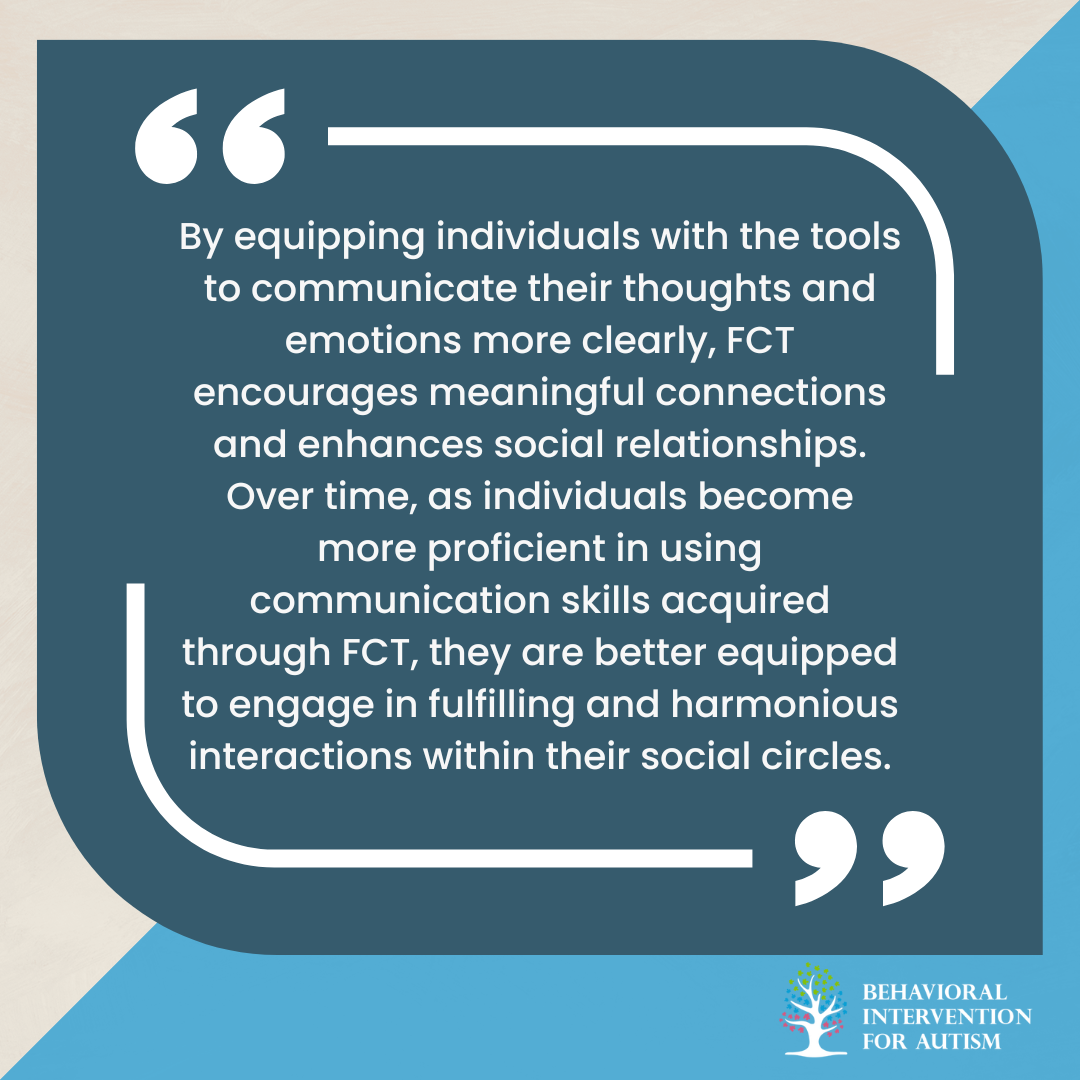
Tone deafness in autism can manifest as challenges in understanding and interpreting social cues, which may lead to difficulties in communication and relationships. It’s essential to recognize these challenges so we can provide the right support. Behavioral Intervention for Autism offers comprehensive ABA programs in Florida tailored to the specific needs of each individual.
Our dedicated team focuses on creating personalized strategies that foster communication skills and enhance social interactions. We believe in empowering our clients and their families, making a positive impact on their daily lives. If you’re interested in learning more about how our programs can help, reach out to us today!