Navigating the workplace can present unique challenges for individuals with autism. Two key areas of difficulty that they may encounter are navigating social interactions and coping with change.
Navigating Social Interactions
Autistic individuals often face challenges when it comes to social interactions in the workplace. They may struggle with understanding social cues, nonverbal communication, and the unwritten rules of workplace etiquette. This can make it difficult for them to build relationships with colleagues, engage in small talk, or navigate office politics.
To help navigate these challenges, it is important to provide clear communication and establish explicit expectations for social interactions. This can include providing written guidelines or protocols for workplace interactions, as well as fostering a supportive and inclusive work environment. Encouraging open and direct communication can also help autistic individuals feel more comfortable expressing their needs and concerns.
Coping with Change
Another challenge that individuals with autism may face in the workplace is coping with change. Many autistic individuals prefer predictable routines and can feel overwhelmed by sudden changes or disruptions to their established work patterns. This can lead to heightened levels of anxiety and stress.
To support individuals with autism in coping with change, it is important to provide clear and advanced notice of any anticipated changes in the workplace. This can help them prepare and adjust to the upcoming changes. Additionally, offering support and accommodations, such as providing visual schedules or written instructions, can help autistic individuals navigate transitions more effectively.
Creating a more inclusive and supportive environment for individuals with autism involves understanding and addressing their unique challenges. Providing necessary support, accommodations, and clear communication enables autistic individuals to thrive in the workplace and reach their full potential.
Stress and Anxiety Management
Managing stress and anxiety is vital for individuals with autism in the workplace. Around 20% of autistic adults have a diagnosed anxiety disorder, which can lead to burnout and negatively impact performance. Implementing relaxation techniques and prioritizing overall well-being can help reduce stress levels and promote a healthier work environment.
Implementing Relaxation Techniques
Relaxation techniques play a crucial role in managing stress and anxiety. These techniques can help individuals with autism regulate their emotions and find a sense of calm in high-pressure situations. Some effective relaxation techniques that can be implemented include:
- Deep breathing exercises: Taking slow, deep breaths can help reduce anxiety and promote relaxation. Encouraging individuals to practice deep breathing techniques during stressful moments can provide them with a coping mechanism to alleviate anxiety symptoms.
- Mindfulness meditation: Mindfulness involves focusing on the present moment and accepting it without judgment. This practice can help individuals with autism become more aware of their thoughts and emotions, allowing them to better manage stress and anxiety.
- Progressive muscle relaxation: This method consists of contracting and subsequently relaxing various muscle groups throughout the body. It helps individuals with autism identify and release tension, promoting physical and mental relaxation.
Encouraging individuals to incorporate these relaxation techniques into their daily routine can provide them with effective coping mechanisms to manage stress and anxiety in the workplace.
Prioritizing Overall Well-being
In addition to implementing relaxation techniques, prioritizing overall well-being is essential for managing stress and anxiety in the workplace. This involves adopting a holistic approach that encompasses various aspects of one’s life. Some strategies for prioritizing overall well-being include:
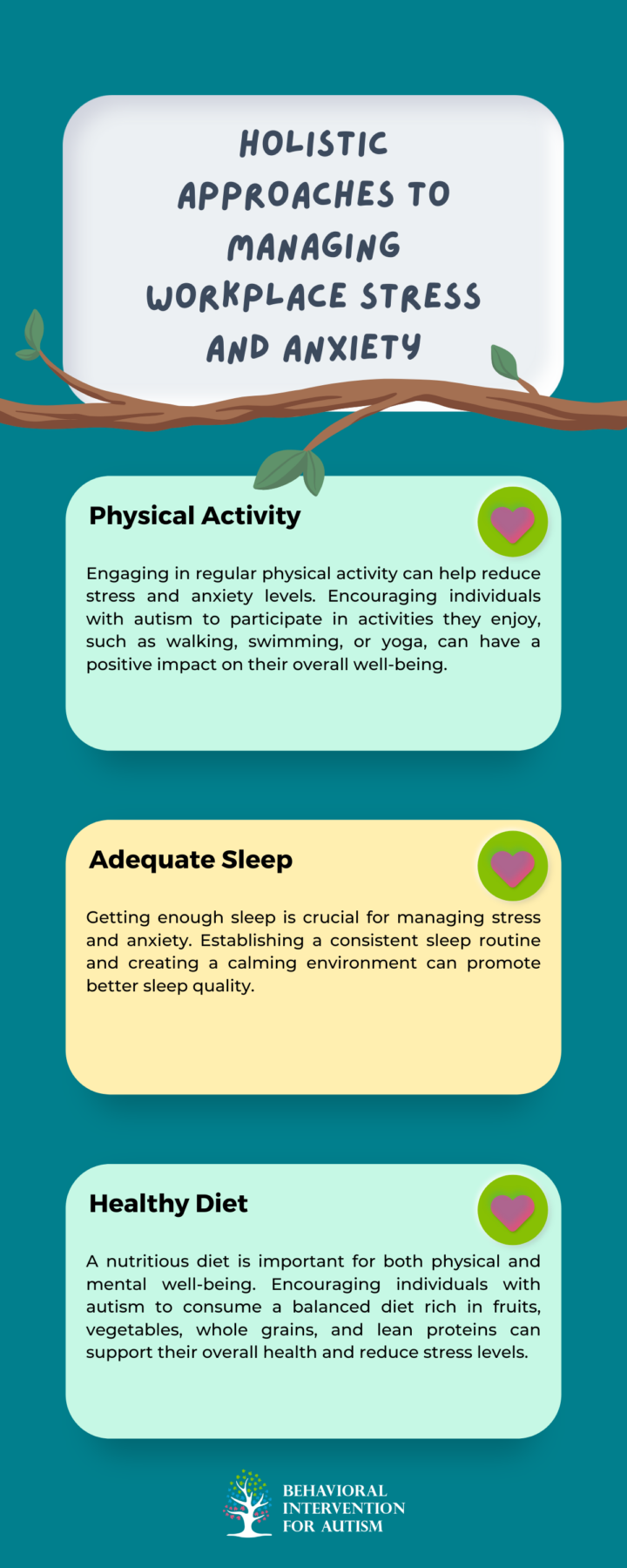
Prioritizing overall well-being allows individuals with autism to manage stress and anxiety more effectively, resulting in improved performance and a more positive work experience. Providing support and creating an inclusive work environment that addresses the unique needs of individuals with autism is essential for fostering their well-being and success.
Workplace Adaptations
For individuals with autism, making adaptations in the workplace can play a significant role in reducing anxiety and creating a supportive environment. By implementing strategies that cater to their specific needs, employers can empower individuals with autism to thrive in their professional lives. Two essential workplace adaptations for individuals with autism include establishing predictable routines and creating supportive work environments.
Establishing Predictable Routines
Individuals with autism often prefer predictable routines and can feel overwhelmed by disorganization or surprises in their work schedule. Establishing clear job duties, requesting advanced notice of schedule changes, and providing comprehensive instructions can help make the workday more predictable and manageable for individuals with autism.
Creating a visual schedule or using task management tools can also aid in establishing routines and providing a clear structure for daily tasks. This visual representation helps individuals with autism understand their responsibilities and navigate their workday more effectively.
Creating Supportive Work Environments
People on the autism spectrum face unique challenges in the workplace, such as feeling overwhelmed by uncomfortable environments, working alongside people who misunderstand or discriminate against them, and struggling with the recruitment and interview process due to social skills being tested. Creating a supportive work environment that fosters understanding and inclusivity is vital for individuals with autism.
To create a supportive work environment, employers can:
- Provide sensitivity training to colleagues to enhance their understanding of autism and promote a culture of acceptance and inclusivity.
- Offer flexible work arrangements, such as adjustable schedules or remote work options, to accommodate the individual’s specific needs and preferences.
- Designate a quiet and calm workspace that minimizes sensory overload, such as reducing bright lights, loud noises, or strong odors.
- Assign a mentor or a buddy system to provide additional support and guidance in the workplace.
These adaptations can help individuals with autism feel more comfortable and supported, allowing them to focus on their work and contribute their unique skills and talents.
Implementing workplace adaptations, such as establishing predictable routines and creating supportive environments, empowers individuals with autism to thrive at work. These changes not only reduce work-related anxiety but also foster a more inclusive and diverse workforce.
To further support this goal, we offer comprehensive ABA therapy in Florida through Behavioral Intervention for Autism. Our dedicated team provides tailored interventions to address specific challenges and improve overall well-being.
Interested in how our services can make a difference for you or your team? Reach out to us today to explore how we can help.